Do you return gastric residual NClex? This question is a critical concern for nurses managing patients with high gastric residual volumes (GRVs). Understanding GRV measurement, implications, nursing interventions, and guidelines is essential for providing optimal patient care. This article delves into the intricacies of GRV management, empowering nurses with the knowledge and skills to effectively assess, intervene, and monitor patients.
Gastric residual volume, the amount of undigested food and fluid remaining in the stomach after a meal, is a crucial indicator of gastrointestinal function. Measuring GRV helps assess gastric emptying, identify potential complications, and guide treatment decisions. Nurses play a pivotal role in measuring GRV, interpreting results, and implementing appropriate nursing interventions.
Gastric Residual Volume (GRV)
Gastric residual volume (GRV) is the volume of stomach contents remaining after a meal or feeding. Measuring GRV is important for assessing the effectiveness of gastric emptying and identifying patients at risk for aspiration pneumonia.
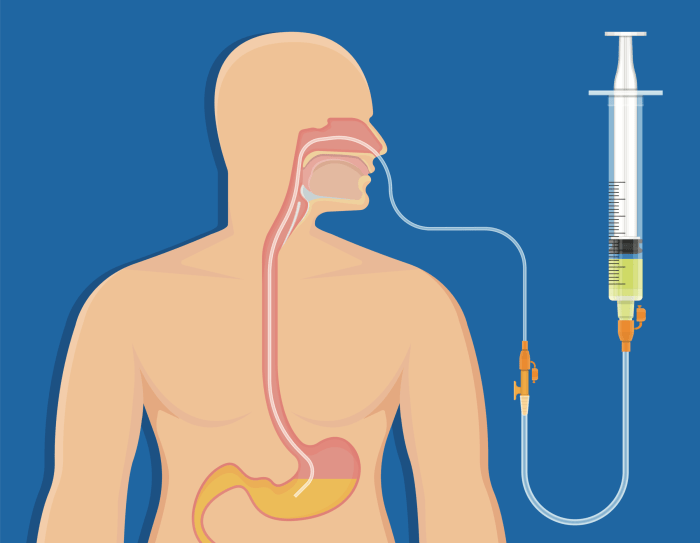
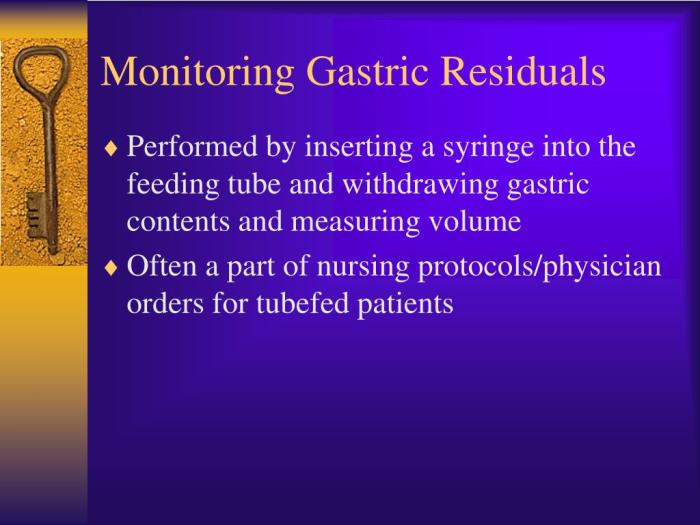
The procedure for measuring GRV involves passing a nasogastric tube into the stomach and aspirating the contents. The aspirated contents are then measured and recorded. A high GRV may indicate delayed gastric emptying, which can be caused by various factors, including gastroparesis, pyloric stenosis, and medications that slow gastric motility.
Implications of a High GRV
- Aspiration pneumonia: A high GRV increases the risk of aspiration pneumonia, which occurs when stomach contents are aspirated into the lungs.
- Delayed gastric emptying: A high GRV may indicate delayed gastric emptying, which can lead to nausea, vomiting, and abdominal pain.
- Nutritional deficiencies: Delayed gastric emptying can interfere with nutrient absorption, leading to nutritional deficiencies.
Nursing Implications
Nursing implications related to gastric residual volume (GRV) are crucial for patient safety and recovery.Nurses play a pivotal role in managing patients with high GRVs by implementing appropriate nursing interventions. These interventions include:
- Monitoring GRV regularly to assess gastric emptying and identify any potential complications.
- Adjusting feeding rates and volumes based on GRV measurements to prevent aspiration and promote optimal nutrient intake.
- Administering prokinetic agents, such as metoclopramide or erythromycin, to stimulate gastric motility and enhance gastric emptying.
- Positioning patients in an upright position or elevating the head of the bed to facilitate gastric emptying and reduce the risk of aspiration.
- Educating patients and caregivers about the importance of monitoring GRV, recognizing signs of high GRV, and adhering to prescribed feeding protocols.
Monitoring GRV is particularly important in specific patient populations, such as:
- Patients with delayed gastric emptying, such as those with diabetes, gastroparesis, or pyloric stenosis.
- Patients receiving enteral nutrition, as high GRVs can indicate feeding intolerance or gastrointestinal complications.
- Patients at risk of aspiration, such as those with impaired gag reflex or decreased level of consciousness.
By monitoring GRV and implementing appropriate interventions, nurses can help prevent complications associated with high GRVs, such as aspiration pneumonia, malnutrition, and electrolyte imbalances.
Role of the Nurse in Patient Education
Nurses play a crucial role in educating patients and caregivers about GRV. This education includes:
- Explaining the purpose of GRV monitoring and its significance in patient care.
- Instructing patients on how to recognize signs and symptoms of high GRV, such as nausea, vomiting, abdominal distension, and decreased appetite.
- Emphasizing the importance of adhering to prescribed feeding protocols and reporting any changes in GRV to healthcare providers.
- Providing written and verbal instructions on GRV monitoring and management techniques, including how to measure and record GRV.
By educating patients and caregivers, nurses empower them to actively participate in their care and minimize the risk of complications related to high GRVs.
Research and Evidence: Do You Return Gastric Residual Nclex
Recent research has focused on improving GRV measurement techniques and developing more effective interventions for reducing GRV.
One study found that using a bedside ultrasound device to measure GRV was more accurate than traditional methods, such as the syringe aspiration method. This study also found that using ultrasound to measure GRV could help to identify patients at risk for aspiration pneumonia.
Another study found that a combination of interventions, including preoperative fasting, elevating the head of the bed, and using a prokinetic agent, was effective in reducing GRV in patients undergoing surgery.
Areas for Further Research
Further research is needed to:
- Develop more accurate and reliable methods for measuring GRV.
- Identify the optimal interventions for reducing GRV in different patient populations.
- Determine the long-term effects of GRV on patient outcomes.
Case Studies
Case studies provide valuable insights into the management of patients with high GRVs and the nursing interventions employed to optimize patient outcomes.
Case Study 1
A 72-year-old male patient with a history of COPD and heart failure was admitted to the hospital with respiratory distress. On admission, his GRV was 250 mL. Nursing interventions included:
- Monitoring the patient’s respiratory status and GRV every 4 hours.
- Positioning the patient in an upright position to facilitate gastric emptying.
- Administering prokinetic agents to enhance gastric motility.
The patient’s GRV decreased to 150 mL within 24 hours, and he was discharged home with instructions to continue monitoring his GRV and seek medical attention if it exceeded 200 mL.
Case Study 2
A 55-year-old female patient with a history of diabetes and gastroparesis was admitted to the hospital with nausea and vomiting. Her GRV was 400 mL. Nursing interventions included:
- Inserting a nasogastric tube to decompress the stomach and reduce GRV.
- Administering antiemetics to control nausea and vomiting.
- Providing nutritional support through parenteral nutrition.
The patient’s GRV decreased to 250 mL within 48 hours, and she was able to tolerate oral feedings. She was discharged home with instructions to continue monitoring her GRV and follow a strict dietary plan.
Nursing Implications
These case studies highlight the importance of assessing GRV in patients at risk for delayed gastric emptying. Nurses play a crucial role in managing high GRVs through appropriate interventions, monitoring, and patient education. Effective management of GRV can prevent complications such as aspiration pneumonia, malnutrition, and electrolyte imbalances.
Guidelines and Policies
Current guidelines and policies for GRV measurement and management aim to ensure accurate assessment, minimize complications, and optimize patient outcomes. These guidelines are based on evidence-based practices and expert consensus.
The rationale for these guidelines and policies includes promoting patient safety, improving patient outcomes, and ensuring consistency in practice. By following standardized guidelines, healthcare providers can reduce variability in GRV measurement and management, leading to better patient care.
Measurement Guidelines, Do you return gastric residual nclex
- Measure GRV before administering enteral nutrition or medications via the enteral route.
- Use a standardized technique, such as the syringe method or gastric aspiration device, to measure GRV.
- Aspirate GRV from the same location in the stomach each time to ensure consistency.
Management Guidelines
- Hold enteral feedings if GRV exceeds a predetermined threshold, typically 250-500 mL.
- Resume enteral feedings gradually when GRV decreases to an acceptable level.
- Consider nasogastric decompression or other interventions if GRV remains elevated despite conservative management.
Areas for Improvement
- Develop standardized protocols for GRV measurement and management across healthcare settings.
- Implement educational programs to improve healthcare provider knowledge and skills in GRV assessment.
- Conduct research to evaluate the effectiveness of different GRV management strategies.
Education and Training
Healthcare professionals, particularly nurses, play a crucial role in the accurate measurement and management of GRV. Therefore, comprehensive education and training programs are essential to ensure nurses possess the necessary knowledge and skills to perform these tasks effectively.
Educational programs on GRV measurement and management should be designed specifically for nurses and tailored to their scope of practice. These programs should encompass both theoretical and practical components to provide nurses with a thorough understanding of the principles and techniques involved.
Target Audience
The target audience for GRV measurement and management education programs includes all nurses involved in the care of patients at risk for aspiration, such as:
- Critical care nurses
- Medical-surgical nurses
- Pediatric nurses
- Geriatric nurses
Learning Objectives
Upon completion of the educational program, nurses should be able to:
- Understand the importance of GRV measurement in preventing aspiration
- Describe the different methods of GRV measurement and their indications
- Perform GRV measurement accurately and safely
- Interpret GRV results and make appropriate nursing interventions
- Educate patients and families about GRV measurement and management
Interactive Activities and Resources
Interactive activities and resources can enhance the learning experience and make the training more engaging. These may include:
- Role-playing exercises to practice GRV measurement techniques
- Case studies to apply knowledge to real-life scenarios
- Simulation training to provide a realistic experience of GRV measurement
- Online quizzes and modules to reinforce learning
- Access to online resources and guidelines for ongoing reference
FAQ Compilation
What is the purpose of measuring gastric residual volume (GRV)?
Measuring GRV helps assess gastric emptying, identify potential complications such as gastroparesis or obstruction, and guide treatment decisions.
What are the implications of a high GRV?
A high GRV can indicate impaired gastric emptying, which can lead to nausea, vomiting, abdominal distension, and aspiration risk.
What nursing interventions are recommended for managing patients with high GRVs?
Nursing interventions include monitoring GRV, adjusting feeding schedules, administering prokinetic medications, and providing patient education.